Cardiomyopathy
Any disease of the heart muscle that interferes with the heart’s ability to pump blood with sufficient force is called cardiomyopathy. Cardiomyopathy develops slowly and may produce no symptoms until the later stages, except when caused by viral infections. It is an uncommon disorder, accounting for only 1 percent of heart disease fatalities. But, it is one of the more common causes of serious heart disease in younger people. Coronary artery disease causes cardiomyopathy in the elderly. Treatment may include medications, implantable devices or, in severe cases, a heart transplant depending upon the type of cardiomyopathy.
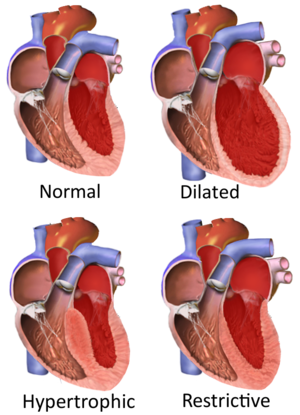
There are three types of cardiomyopathies including :
9,600+
Happy Patients
10
Qualified Doctors
500+
Successful Surgeries
100+
Insurance Partners
Cause of the cardiomyopathy is unknown in most cases. However, doctors are able to identify some contributing factors in some people. Possible causes of cardiomyopathy include:
There is a lot of variations in the symptoms of cardiomyopathy.
Possible symptoms of dilated cardiomyopathy:
Possible symptoms of hypertrophic cardiomyopathy are generally same as the symptoms of dilated cardiomyopathy. Rarely the first symptom may be fainting or even sudden death. It can also cause heart attack, usually during exercise.
Possible symptoms of restrictive cardiomyopathy are fluid accumulates in the legs and abdomen. This condition also can cause shortness of breath, especially during exertion.
Irrespective of type of cardiomyopathy you have, signs and symptoms tend to get worse unless treated. This worsening happens quickly in certain people, while in others, cardiomyopathy may not worsen for a long time.
On a doctor visit, a physical examination of the patient will be conducted. A personal and family medical history will be taken, and patient asked about symptom occurrence — for example, whether exercise brings on your symptoms. You may need to undergo several tests if your doctor thinks you have cardiomyopathy, to confirm the diagnosis. These tests may include:
Many other blood tests, including those to check your kidney function and look for anemia and thyroid problems, might be done. Your doctor may order by checking your iron level. Increased iron in blood may indicate an iron overload disorder called hemochromatosis. Accumulating too much iron in your heart muscle can weaken it and cause cardiomyopathy.
Other conditions arising due to cardiomyopathy are:
The management of cardiomyopathy aims to reduce your signs and symptoms, prevent your condition from worsening, and decrease your risk of complications. Treatment varies by which of the major types of cardiomyopathy you have.
Dilated Cardiomyopathy
In this condition, your doctor may recommend medications, surgically implanted devices or a combination of both. The medications you may be prescribed include:
In some cases, a special pacemaker is implanted that coordinates the contractions between the left and right ventricles (biventricular pacing). Drug therapy or an implantable cardioverter-defibrillator (ICD) may be options in people who may be at risk of serious arrhythmias.
Hypertrophic cardiomyopathy
In this condition, your doctor may recommend beta blockers to relax your heart, slow its pumping action and stabilize its rhythm. These medications also calcium channel blockers, such as verapamil. In hypertrophic cardiomyopathy, medications are often the preferred treatment. You may need surgery or a medical device to treat your condition if medications don’t work. Options include:
Septalmyectomy.It is a type of an open-heart operation in which the surgeon removes part of the thickened, overgrown heart muscle wall (septum) that separates the two bottom heart chambers (ventricles). This removal improves blood flow and reduces mitral regurgitation. Most patients improve with this surgery and have no further symptoms.
Septal ablation.In this treatment, a small portion of the thickened heart muscle is destroyed by injecting alcohol through a catheter into the artery supplying blood to it. There are possible complications with this procedure, including heart block — a disruption of the heart’s electrical system — which requires implantation of a pacemaker. Although the long-term success of this procedure isn’t yet known, it’s becoming more commonly used.
Pacemaker implantation.In this procedure, a small electronic device is inserted under your skin that sends electrical signals to your heart to monitor and regulate your heartbeat. This procedure is generally done under local anesthesia and typically takes less than three hours. But, this procedure is not as effective as surgical options, but it’s sometimes used in older people who want to avoid more invasive procedures. Implantable cardioverter-defibrillator (ICD).In this procedure, a pager-sized device is implanted in your chest like a pacemaker. This device continuously monitors your heartbeat. In case a life-threatening arrhythmia is detected, the ICD delivers precisely calibrated electrical shocks to restore a normal heart rhythm. In patients at risk of a sudden cardiac death because of abnormal heart rhythms, this device is very useful.
Restrictive cardiomyopathy
Pacemaker implantation.In this procedure, a small electronic device is inserted under your skin that sends electrical signals to your heart to monitor and regulate your heartbeat. This procedure is generally done under local anesthesia and typically takes less than three hours. But, this procedure is not as effective as surgical options, but it’s sometimes used in older people who want to avoid more invasive procedures. Implantable cardioverter-defibrillator (ICD).In this procedure, a pager-sized device is implanted in your chest like a pacemaker. This device continuously monitors your heartbeat. In case a life-threatening arrhythmia is detected, the ICD delivers precisely calibrated electrical shocks to restore a normal heart rhythm. In patients at risk of a sudden cardiac death because of abnormal heart rhythms, this device is very useful.
Heart transplant and ventricular assist devices (VADs)
A heart transplant may be an option if you have severe cardiomyopathy and medications can’t control your symptoms. Even people who are critically ill may have a long wait before having a heart transplant because of the shortage of donor’s hearts. A mechanical heart assist device can help In some patients who are critically ill as they wait for an appropriately matched donor. These devices, known as ventricular assist devices (VADs), can help blood circulate through your heart for months or even years.VAD therapy could be a long-term treatment option for some people who aren’t candidates for a heart transplant.
Lifestyle measures
Choose the following lifestyle measures to help you manage cardiomyopathy:
Specific recommendations will depend on the type of cardiomyopathy you have.
Prevention
Generally, you can’t prevent cardiomyopathy in many cases. If you have a family history of the condition, consult a doctor. If cardiomyopathy is diagnosed early, treatments may prevent the disease from worsening. Preventing the diseases that cause cardiomyopathy is the best to prevent it. Know your risk factors for coronary artery disease and modify those risks early in life. You can reduce your risk for coronary artery disease by:
Contact your doctor for evaluation if you have any family members with inherited cardiomyopathy.